Frontier science
B cells are the new frontier in cancer immunology. Clinically, B cells is associated with improved survival outcomes in most cancers, including breast, sarcoma, HNSCC, cervical, melanoma, and other solid tumors¹¯³. B cells can mount an immune response against cancer cells via multiple mechanisms:
Immune cell recruitment and organization. B cells release different molecules that can recruit immune cells and also organize them into specialized structures called tertiary lymphoid structures (TLS). The presence of TLS in the tumor is associated with better prognosis.
Prime, shape and amplify T cell response. B cells act as antigen presenting cells (APCs) to T cells. Naive B cells do not require antigen presentation to internalize antigens, and hence act as one of the earliest APCs. Activated B cells also secrete IFNs that can stimulate the immune response.
Direct antibody effects. This is the best-known mechanism via which a B cell exerts an immune effect. Upon activation, B cells switch to antibody-secreting plasma cells and memory B cells. Antibodies can bind to cancer cell antigens (surface proteins or cell surface receptors), resulting in internalization of the bound complex and degradation and loss of cellular signaling and function.
Activate the innate immune system. Naive B cells produce low specificity IgM antibodies that can recognize a broad array of antigens in the tumor, and recruit innate immune cells, including macrophages, NK cells, etc. This acts as one of the first line of defense in our immune system.
Compared with current immune checkpoint inhibitors that activate either innate immune cells or T cells, recruiting a B cell immune response in the tumor activates both T cells and innate immune cells against the tumor, i.e. a 360 degree immune response. Activating B cells therefore holds the promise of greater antitumor efficacy than current immune checkpoint inhibitors.
How do B cells kill cancer cells?
B cells exert a 360 degree immune response, activating both innate and adaptive immune cells.
In preclinical studies, treatment with AT-1965 regressed 4T1 breast cancers, resulting in an ORR of >80% in this hard to treat tumor.
AT-1965 inhibits CMTR2, a novel target in cancer cells, converting cancer cell RNA into viral-like RNA. Cancer cells produce large amounts of RNA as they are transcriptionally overactive, and start shedding these viral-like RNAs. This triggers the intrinsic function of B cells to mount an immune response against this viral signature.
High levels of CMTR2 in the tumor is associated with poor outcomes. Hence inhibiting CMTR2 in cancers can improve outcomes, especially in tumors that exhibit improved survival association with B cell infiltration.
How does AT-1965 work?
High levels of CMTR2 in breast cancer is associated with poor survival outcomes.
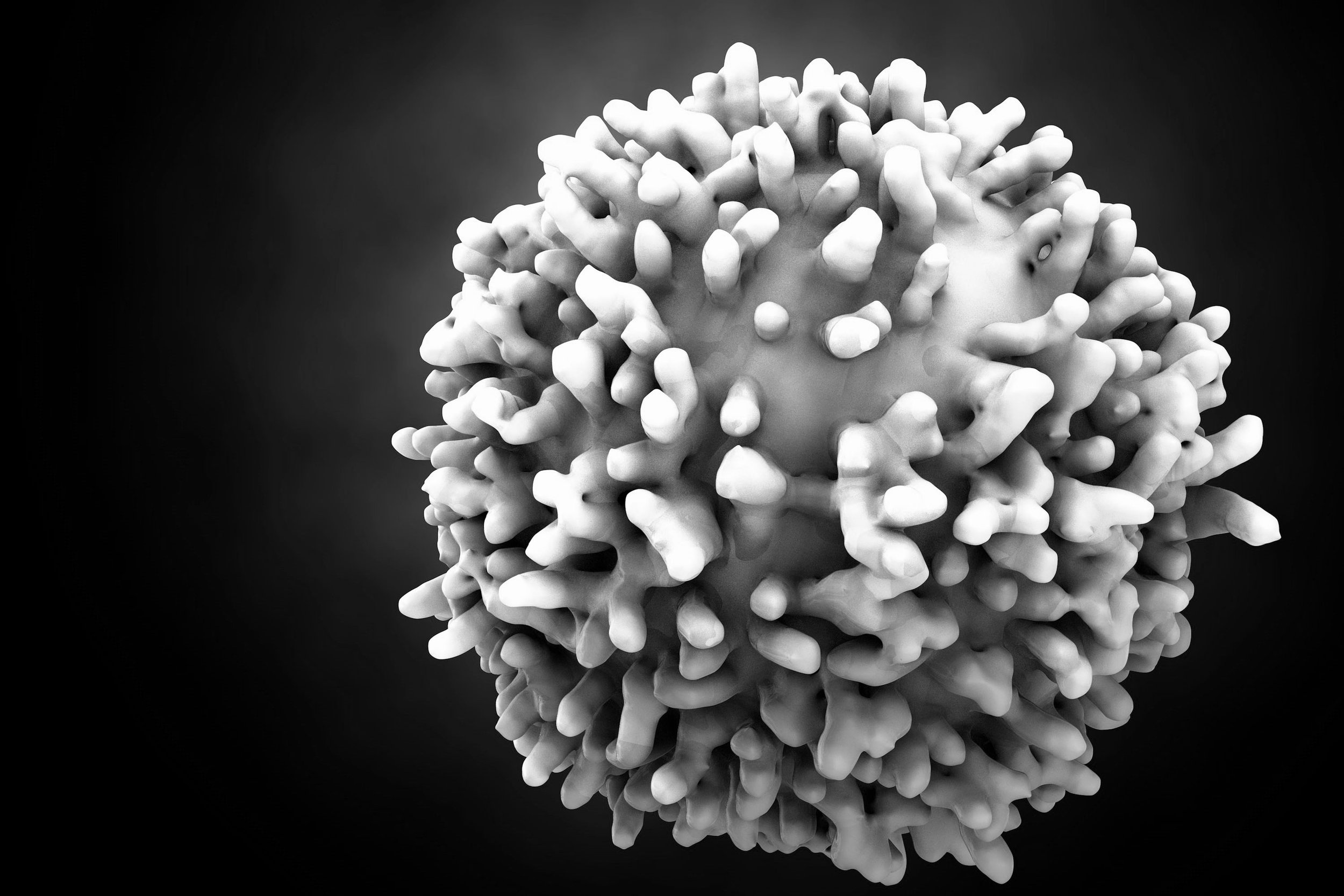
Image shows the putative structure of CMTR2 with AT1965 (yellow) docked in the active site.
¹Nature. 577, 549-555 (2020); ²Nature. 597, 274-278 (2021); ³Cancer Cell. 41(3):466-489 (2023)




